β-blockers: Personalized medicine
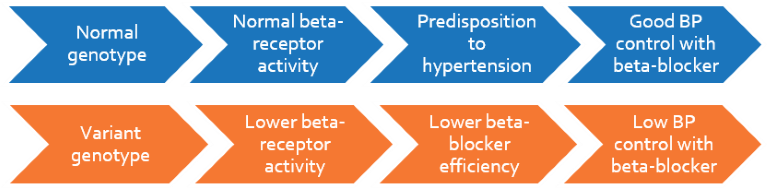
30 to 60% of hypertensive patients who are on beta-blocker monotherapy fail to respond adequately. This variation in response is accounted for by a genetic polymorphism in the ADRB1 gene, which encodes the adrenergic beta-receptor type-1 to which the drug binds to exert an antagonistic effect. The ADRB1 variant (1165C>G) inherently confers a beta-blocker-like effect, thereby making beta-blocker treatment redundant. Patients with wildtype ADRB1 will benefit from beta-blocker therapy, while patients with one copy of variant may need combination therapy. Individuals with two copies of variant are largely resistant to beta-blockers.
Clinical Significance
- 1 out of 3 Asians have a variant ADRB1 genotype and may have lower benefits from beta-blocker treatment
- ADRB1 wildtype genotype is associated with an increased risk of developing hypertension
- Patients with wildtype genotype benefit from beta-blocker therapy and have lower risks of cardiovascular complications
- Patients with variant genotype respond poorly to beta-blockers and may need additional medication to prevent cardiovascular complications
Personalize Beta-blocker Test
Patients will be genotyped for ADRB1 1165C>G to assess their response to beta-blockers. Wild type individuals may benefit from beta-blocker therapy. For individuals that may not benefit from beta-blockers, alternative antihypertensive medications may be indicated.
Beta-blockers improve survival rate and decrease hospitalization in wildtype ADR1 patients – BEST trial, Liggett SB et al. 2006, Proceedings of National Academy of Science of USA
- Survival rates, in terms of mortality and hospitalization, were analyzed in 1040 class III/IV heart failure patients randomized to receive bucindolol or placebo and followed-up over 18 months
- In variant patients, no significant difference in clinical response between bucindolol or placebo was seen
- However, wildtype homozygotes treated with bucindolol vs. placebo had:
-38% reduction in mortality (p=0.03)
-34% reduction in hospitalization (p=0.004)
- No genotypic association was evident in the placebo group, indicating little impact on the normal course of heart failure
Relationship between ADRB1 genotypes and beta-blocker dosage – Heart Failure (HF)-ACTION study, Fiuzat M et al. 2013, European Journal of Heart Failure
- The relationship between beta-blocker dose and ADRB1 genotype was assessed in 957 heart failure patients with systolic dysfunction
- Wildtype homozygotes given a low dose of beta-blocker had a two-fold increased risk of death compared to those given a higher dose (hazard ratio 2.09; p=0.015)
- To achieve similar response, patients with two copies of wildtype allele require a higher dose than heterozygotes
Genotypic influence on beta-blocker mediated Left Ventricular Ejection Fraction (LVEF) increase, Chen L et al. 2007, Pharmacogenetics and Genomics
- In 135 patients with non-ischemic cardiomyopathy and chronic heart failure, changes in LVEF before and 1.5 years after carvedilol treatment were correlated with ADRB1 genotype
- A greater improvement in LVEF was seen in wildtype homozygotes compared with variant allele carriers (p<0.001) upon carvedilol therapy
Variant ADRB1 offers protection from essential hypertension (EH), Wang H et al. 2013, Molecular Biology Reports
- Meta-analysis in 5088 EH patients and 6515 controls determining association of ADRB1 gene variant
- The variant allele frequency was significantly lower in the EH group than in the controls (OR = 0.89, p = 0.04) suggesting that the wildtype allele may confer predisposition for EH