Male infertility: FSH and Personalized medicine
Men with infertility and where both partners are infertile will benefit from this test. It genotypes the patient for these two variations in FSHR and FSHB and classifies him for infertility treatment by FSH  administration. The report will indicate recommendations for improving sperm parameters in men with variants, which may improve outcome of both natural reproduction as well as ART.
administration. The report will indicate recommendations for improving sperm parameters in men with variants, which may improve outcome of both natural reproduction as well as ART.
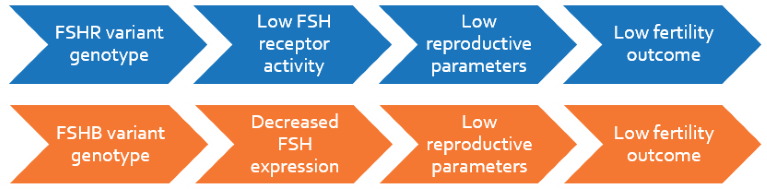
Follicle stimulating hormone (FSH) is important for male reproductive function and mediates its action by binding to the FSH receptor (FSHR) expressed on Sertoli cells. A common variation of FSHR (2039A>G), prevalent in 41% of the population, results in decreased receptor function. This affects spematogenesis by decreasing sperm count, motility and testes volume.
FSHB encodes the beta-subunit of FSH, which binds to FSHR and mediates hormonal action. A variation in the gene promoter (-211G>T), prevalent in 8% of population and markedly higher among infertile men, leads to decreased FSH expression and activity. This variation is similarly associated with decreased testicular volume, sperm concentration and motility.
Clinical Significance
- Almost 1 in 2 men, and a much higher proportion of infertile men, carry variant FSHR and FSHB
- Men with these variants will benefit from short-term FSH treatment
- Such treatment is known to significantly improve sperm parameters to enable fertility
Indications
- Azoospermia, non-obstructive
- Oligozoospermia (<20 million sperms/ml)
- Idiopathic infertility
 Oligozoospermia to normozoospermia conversion by FSH therapy in FSHR variant men, Selice R et al. 2011, International Journal of Andrology
Oligozoospermia to normozoospermia conversion by FSH therapy in FSHR variant men, Selice R et al. 2011, International Journal of Andrology
- Clinical trial of 70 men with normal FSH levels and oligozoospermia treated with 150 IU FSH thrice a week for 3 months, and 35 normozoospermic men
- Significant increase in total sperm count, sperm concentration, forward motility, percentage of normal morphology forms and total motile sperm were seen in FSHR variant men
- Men without FSH variation did not show improvement in sperm parameters
Additive effect of FSHR and FSHB variants on sperm parameters and testicular volume, Tuttelmann F et al. 2012, Journal of Clinical Endocrinology and Metabolism
- A meta analysis of 3017 men found strong negative association in FSHB variant men for:
‐bitesticular volume (p=0.0000028)
‐sperm concentration (p=0.00000002)
- A cohort study of 1213 men attending an infertility clinic
- Bi-testicular volume was significantly negatively associated with men carrying 2 copies of the variant
- Mean sperm concentration was significantly lower in men carrying the variant allele
- Total sperm count was significantly decreased in men with variant FSHB
FSH therapy doubles sperm count and makes FSHB variant infertile men normozoospermic, Ferlin A et al. 2011, Fertility and Sterility
- A cohort study in 1246 men referred for fertility evaluation
- FSHB variant carriers had significantly lower levels of:
‐serum FSH, 3.3 ± 2.5 IU/L (p = 0.0026)
‐sperm count, 10.4 ± 11.6 *106/ml (p=0.21)
‐percentage of motile sperms, 28.5 ± 6.2%
- Significant improvement of male reproductive parameters were observed in variant carriers upon FSH therapy with 150 IU rhFSH thrice a week for 3 months:
‐doubling of sperm count was observed in
- 100% of variant homozygous carriers (TT)
- 65% of variant heterozygous carriers (GT)
‐conversion to normozoospermia was observed in
- 66.7% of variant homozygous carriers (TT)
- 25% of variant heterozygous carriers (GT)
‐motile sperm count also increased significantly by
- 58.3% in variant homozygous carriers (TT)
- 44.2% in variant heterozygous carriers (GT)
FSHR variant men have significantly poorer reproductive parameters, Lindgren I et al. 2012, Pharmacogenetics and Genomics
- A cohort study involving 313 young men aged 17-20 years
- Significantly lower reproductive parameters were observed in carriers of both one and two copies of variant alleles:
‐sperm concentration (p=0.04)
‐sperm count (p<0.0001)
‐reduced testes volume (p=0.02)