Female infertility: FSH and personalized medicine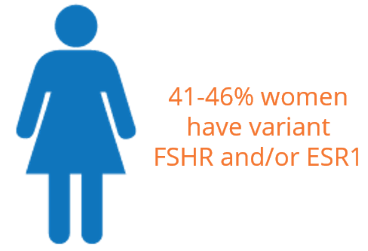
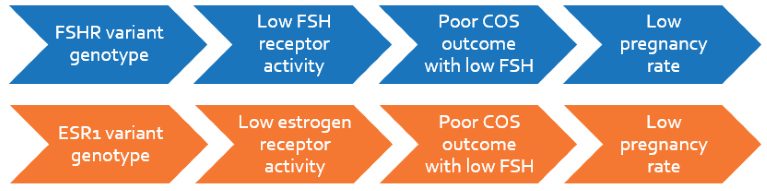
Follicle stimulating hormone (FSH) is responsible for the growth and recruitment of immature ovarian follicles in women. It acts by binding to the FSH receptor (FSHR) present on ovarian and uterine cells. A common variation of FSHR (2039A>G), prevalent in 41% of the population, binds poorly to FSH and results in reduced receptor function. This affects oogenesis in terms of reduced antral follicles, lower number of oocytes, longer stimulation period and lower maturing follicles translating into poor pregnancy outcome. Controlled Ovarian Stimulation (COS) in these women are significantly more successful with higher doses of FSH yielding higher antral follicle count and mature follicles, and improved oocyte quality and number of oocytes retrieved, resulting in better pregnancy outcome.
Estrogen plays a key role in folliculogenesis and embryo implantation by binding to estrogen receptors (ESR1 and ESR2). A variation in ESR1 (453-397T>C), found in 45% of women, affects estrogen receptor activity, and thus implantation outcome. Women with variant allele have lower number of follicles, mature oocytes, and good quality embryos resulting in poor COS outcome. Estrogen biosynthesis being regulated by FSH, exogenous FSH administration increases the hormone, thereby overcoming reduced ESR1 activity in these women. This may translate into improved COS outcome during IVF, ICSI and other oocyte retrieval procedures.
Clinical Significance
- 41% of women in the general population, and >75% of women undergoing IVF, have variant FSHR
- 45% of women in the general population have variant ESR1
- Women with these variants are poor responders in COS with lower oocyte recovery
- A higher dose of FSH in these women significantly improves COS outcome in terms of oocyte recovery, primary antral follicles, shorter stimulation period and higher pregnancy rate
Female FSH panel
The test is suitable for all women undergoing or contemplating ART involving COS, such as IVF and ICSI. The test will genotype women for FSHR (2039) and ESR1 (453-397) variations, classifying them into responder type for COS outcome. The report will indicate recommendations for altering FSH levels to improve COS outcome which can translate into an increased pregnancy rate in women with variation.
 Indications
Indications
- Controlled Ovarian Stimulation (COS)
- Prior to IVF, ICSI, or any oocyte-retrieval procedure
- Normovulatory, oligovulatory and anovulatory women contemplating ART
- Prior to ART for tubal factor infertility, endometriosis or PCOS
FSHR Variant (2039A>G) associated with poor COS outcome, Yan Y et al. 2013, PLoS One
- Prospective cohort study of 450 women participating in an IVF program
- Significantly higher exogenous FSH was used for stimulation depending on variant copy number: women with two variant copies > one variant copy > zero variant copies (p < 0.05)
- The number of days required for stimulation was significantly higher in women with two variant copies compared to women not carrying the variant allele (p < 0.05)
In normovulatory women, FSHR variant in an ovarian donor program associated with poor COS outcome, Lledo B et al. 2013, Pharmacogenetics and Genomics
- Cohort study with 145 normovulatory fertile women participating in an ovarian donor program including 355 COS cycles
- Significantly higher levels of gonadotropin was used for oocyte stimulation in women bearing the variant FSHR allele versus women not carrying the variant allele (p < 0.001)
- FSHR variants were also significantly different from women with no variant allele in:
‐lower antral follicle count (p = 0.0001)
‐number of eggs retrieved (p < 0.001)
ESR1 variant associated with low follicular maturation, fertilization rates and embryo quality, Ayvaz O et al. 2009, Journal of Assisted Reproduction Genetics
- Clinical cohort study of 104 patients and 107 controls
- Maturation rates of oocytes was significantly lower in carriers of 2 variant copies than those without variant allele (82% vs. 94%, p < .001)
- Fertilization rates of oocytes was significantly lower in carriers of 2 variant copies than those with wildtype allele (60-71% vs. 87%, p < 0.001)
- The number of good quality embryos (grades 1 and 2) was significantly lower in carriers of 2 variant copies than those with wildtype allele (8 vs. 10, p < 0.001)
- On the other hand, the number of poor quality embryos (grades 3 and 4) was significantly higher in carriers of 2 variant copies than those with wildtype allele (6 vs. 7.5, p < 0.001)
In normovulatory women, ESR1 variant associated with poor ovarian stimulation and fertilization outcome, Altmae S et al. 2007, Molecular Human Reproduction
- Clinical study of 159 normovulatory infertile women
- Ovarian stimulation developed 5.3 more follicles in women with wildtype allele as compared to those with two variant copies (p = 0.033)
- Women with wildtype allele also had a higher oocyte retrieval rate than ones without wildtype allele (p = 0.05)
- Amount of FSH required for COS was significantly different depending on the number of variant copies: 2 variant copies > 1 variant copy > 0 variants (p < 0.05)
Clinical pregnancy rate was also considerably higher in women with wildtype genotype and heterozygotes compared to women with two variant copies